The brewing uncertainty of 2020 served as the backdrop for Michael Brooks’ and Déjà Curry’s son, Vincent’s, care journey. Before the calendar turned to the year remembered for the first wave of the COVID-19 pandemic and nationwide civil unrest, Déjà received alarming news during an ultrasound with experts at Park Nicollet maternal-fetal medicine. She learned her unborn child had a possible hole in his heart and a potentially life-threatening condition called a diaphragmatic hernia (DH).
Vincent had a hole in the dome-shaped muscle in his chest called the diaphragm. The diaphragm helps us breathe and also serves as a critical barrier to separate our lungs from our stomach and intestines. But due to the hole, Vincent’s developing organs were being pushed up into his lungs.
“I thought ‘how can this be happening to us.’ There was a lot of fear and uncertainty with many mixed emotions and unknowns,” Déjà said.
Fetal care and monitoring
Déjà was referred by Park Nicollet to the Midwest Fetal Care Center (MWFCC), a collaboration between Allina Health and Children’s Minnesota. Here, she met with a multi-disciplinary team of highly trained maternal-fetal medicine experts including Dr. Saul Snowise, medical director of the MWFCC; Dr. Joe Lillegard, the head of open fetal surgery at the MWFCC; and Dr. James Fisher, pediatric surgeon at Children’s Minnesota. The team closely monitored the mother and son with frequent ultrasounds until it was time for her to deliver.
Vincent’s arrival
On Jan. 9, 2020, Déjà delivered Vincent in Minneapolis at The Mother Baby Center, a partnership between Allina Health and Children’s Minnesota. The Kid Experts® in the Children’s Minnesota neonatology program and its Level IV neonatal ICU (NICU) – the highest level designated by the American Academy of Pediatrics – immediately got to work. Vincent needed surgery to repair his diaphragm.
“We had an amazing team of doctors and nurses we became to know and trust,” Déjà said. “Vincent’s team from the NICU were all so incredible and like angels watching over him.”
Vincent spent nearly the entire first five months of his life in the NICU and Children’s Minnesota’s cardiovascular department. The latter is where he received specialized life-saving care for his heart and lungs.
ECMO
Vincent’s intestines and liver had caused his lungs to be underdeveloped and had compressed his heart. This contributed to the newborn having major difficulty breathing on his own.

Vincent now required life support to survive using a special machine called extracorporeal membrane oxygenation (ECMO). Vincent’s primary physician in the NICU, Dr. Lia Gravari, director of neonatal ECMO at Children’s Minnesota, and her team closely monitored and cared for the baby. ECMO uses a pump that works like the heart to pump blood from Vincent’s body through an artificial lung to add oxygen to his blood and remove carbon dioxide. It then sends the blood back to his body.
Vincent also experienced a brain bleed that required surgery and had a stroke.
“I remember being so helpless and afraid, crying almost every day driving to and from Children’s Minnesota,” Déjà said while also reflecting on the world around her at the time in early 2020.
Déjà shared how Vincent’s big sister only got to see him once in the hospital due to COVID safety protocols. So, the child life team sent her materials at home to help her understand why her brother was away. Déjà also praised other non-clinical programs at Children’s Minnesota that supported her family such as the music therapy team.

‘A miracle and more than amazing’
May 8, 2020, was the day Déjà and her family had been waiting for – after nearly five months in the hospital – baby Vincent no longer needed ECMO or inpatient care and he could go home. During this time, the murder of George Floyd and the civil unrest that followed sparked in Minneapolis and around the world.
“I will never forget the National Guard being there to protect the children and staff, or passing parts of the city that were on fire while attending follow-up visits for Vincent,” Déjà said.
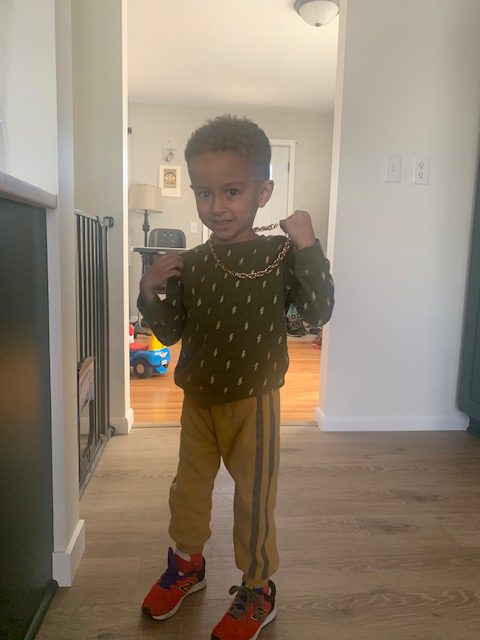
Four years later, Vincent is thriving, and his mom says he’s defied all odds by not having any serious complications from his brain bleed and stroke. However, he still sees specialists in physical therapy, pulmonology and gastroenterology.
“Our major struggle currently is digestion, but we are trying different things and hoping we soon get that under control,” Déjà said.
Like most 4-year-old kids, Vincent loves to play with cars, learn, sing and dance. He hopes to play soccer someday soon too.
“Vincent is a miracle and more than amazing,” Déjà said. “He astonishes me every single day, whether he is learning to jump, run or using vocabulary I don’t even use.”
A Wall of Fame-worthy story
While Vincent’s story is just beginning, the impression he made at Children’s Minnesota will last forever. He’s now part of the Stories of Hope wall in the Minneapolis NICU where his picture joins many of other inspiring patients’ photos who are now thriving.
“This was an absolute honor when we were asked if he could be added to the wall,” Déjà said. “I remember walking up and down those halls several times daily; sad or very angry at times and I would always stop to take time and read other patient’s stories on the wall, it gave me SO much hope!”
Now, Vincent’s story will inspire hope in future NICU patient families walking those same halls.