Cutting edge findings from the Children’s Minnesota Cancer and Blood Disorders research team and collaborators show variants in the deep intronic (noncoding) region of DICER1 may increase risk for tumor development in kids and young adults. DICER1 is a key gene involved in gene expression; pathogenic variants in DICER1 increase risk for pleuropulmonary blastoma, ovarian Sertoli-Leydig cell tumors, thyroid nodules and thyroid cancer and a spectrum of other tumors. This analysis, published in the Journal of Clinical Oncology-Precision Oncology, was led by pediatric oncologists, Kris Ann Schultz, MD, and Yoav Messinger, MD, and Paige Mallinger, MS, senior clinical research coordinator, along with collaborators from the University of Texas Southwestern Medical Center and others.
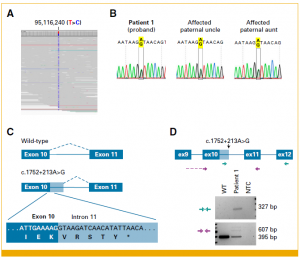
Individuals and family members were enrolled in this study if they had a medical history with a suspected germline variant in DICER1 but negative clinical testing. Their blood and tumor samples were analyzed. With additional testing, variants deep in the intronic region were found and confirmed to alter Dicer function. These findings, not generally detected by standard clinical testing, may allow improved assessment of tumor risk in patients and family members. Improved understanding of risk makes earlier diagnosis possible and results in better outcomes for kids and their families with or at risk for DICER1-related cancers.
The research was conducted using the International PPB/DICER1 Registry and with the help of its members. The registry was founded at Children’s Minnesota in 1987 in partnership with Washington University-St. Louis and now collaborates with many institutions worldwide. The registry now includes more than 1,100 individuals from 47 states and 49 countries worldwide. Its mission is to improve outcomes for children and adults with pleuropulmonary blastoma (PPB), Sertoli-Leydig cell tumor and other DICER1-related cancers. Earlier this year, the registry team published outcomes of the largest ever cohorts of children with Type I and Ir and Types II and III pleuropulmonary blastoma (PPB).
Learn more about our R01/R37 research in DICER1 biomarkers and our surveillance article.
Connect with us
To connect with one of our cancer and blood disorder program kid experts, call the Children’s Minnesota Physician Access Line.
Doctors and healthcare providers call for 24/7 patient referral, admission and neonatal transport assistance. Learn more.